
457: Ask David: Chasing, Sadness as Celebration, and Autism
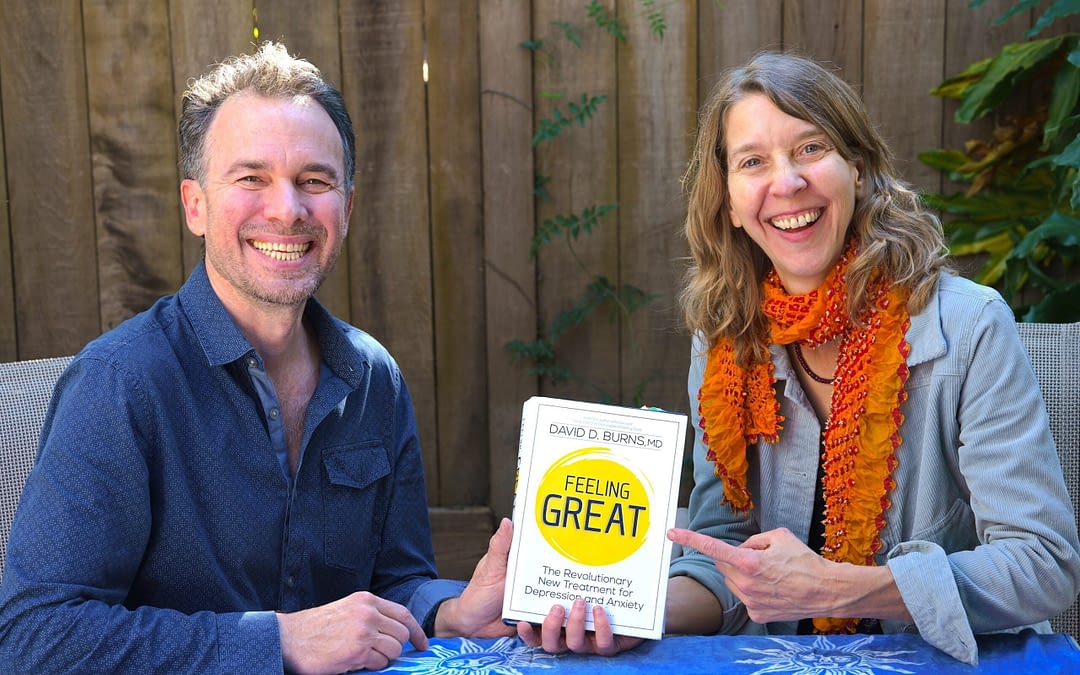
Dr. Matt May, Dr. Rhonda Barovsky, and David answer your questions on the fear of being alone or abandoned, and how to live with someone who is depressed and irritable!

Dr. Matt May, Dr. Rhonda Barovsky, and David answer your questions on the fear of being alone or abandoned, and how to live with someone who is depressed and irritable!

Here’s your chance to learn the powerful TEAM tools for rapid change from two amazing experts! Join the popular Feeling Great Book Club, starting September 15th and 17th, led by brilliant teachers: Dr. Brandon Vance and Dr. Heather Clague.

Learn from Dr. David Burns and Dr. Jill Levitt! Join us for a FREE, two-hour webinar on one of the most common causes of stress and feelings of inadequacy–perfectionism. This live, practical training will equip you with powerful, research-backed techniques!

Dr. Matt May, Dr. Rhonda Barovsky, and David answer your questions on the fear of being alone or abandoned, and how to live with someone who is depressed and irritable!

Discover two powerful stories: one about the hidden damage of “Should” statements—and another about the brilliant but tormented philosopher Ludwig Wittgenstein. These videos explore how distorted thinking fuels emotional pain—and how insight can bring healing.